
The root-cause disease: Chronic inflammation
Jul 19, 2023Various studies and research papers have shown that chronic inflammation is a recurrent factor in most diseases that have become epidemics today.
Chronic pain, obesity, anxiety, diabetes, heart disease, depression, stroke, migraine, thyroid problems (such as Hashimoto’s disease), attention deficit disorder, ADHD, gastritis, dermatitis, Alzheimer’s disease, cancer and a long list of other diseases present a state of unresolved inflammation in almost every instance.
What is inflammation and how does it work? (In a nutshell)
Inflammation eliminates the root cause of cellular lesions or damaged cells and tissues and kick-starts tissue recovery.
Inflammation starts when the body releases cytokines (protein molecules that act as communication signals between immune system cells and different organs and tissues). These act as emergency signals, carry nutrients, hormones and immune system cells to the location of the wound. To make this process easier, arteries dilate, while capillaries become more permeable to ensure that the cells that need to perform the “repair” function are able to access the wounded area. From there, the immune system cells perform their duties until the problem is solved.
What is chronic inflammation?
Inflammation is described as “chronic”, when the inflammatory process never reaches a phase of conclusion (never Terminates as outlined by the Integrative Functional Patterns cycle), such as when active inflammation and tissue destruction, with attempts at healing, co-exist for a length of time.
How does inflammation start? Gut, Stress, Trauma, Food
The gut is composed of a semi-permeable coating that is incredibly vast and intricate. Its degree of permeability changes in response to various chemically mediated conditions.
For example, when cortisol (popularly known as the “stress hormone”) is elevated due to the stress caused by an argument or by trauma, or when we introduce an excessive amount of inflammatory foods such as sugar and trans fats, the intestine walls becomes immediately more permeable.
Bad posture, caused by feeling tense and being in a hurry, as well as thoughts that are constantly negative, also favour lengthy inflammatory states. [If you want to explore different psychosomatic mechanisms you can find many other articles and videos in our blog.]
When the intestine walls are repeatedly damaged (by stress and constant conflict, inadequate nutrition, irregular emotions etc.), cells in the gut become unable to carry out their job correctly and cannot to elaborate and use nutrients or produce the key substances required for adequate digestion that is thus compromised.
What are the defence processes for the gut and immune system?
Immune system defence is composed of various barriers.
- The first barrier is the gut microbiome, also known as gut flora, and amounts to the bacteria and microorganisms that live in the body’s mucous membranes, especially in the digestive tract and in the gut. The microbiome performs a critical role in immune defence producing a series of key substances (such as short chain fatty acids) that regulate homeostasis and pathogen defence processes.
- The gut mucous membrane represents a second barrier: a single layer of epithelial cells that separate the gut lumen home to bacterial flora in the gut epithelium. Mucus stops large particles from coming into contact with the epithelial cell layer, enabling the passage of small molecules.
- A third barrier is represented by the gut epithelium, a layer of epithelial cells that cover the intestine and that protect it but also manage the absorption of nutrients and other substances.
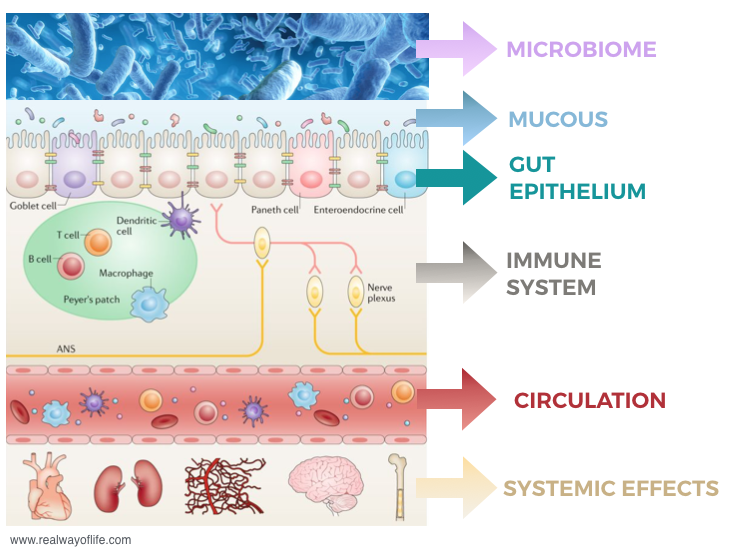
Below all these layers we find the immune system itself, composed of a series of cells whose role it is to defend the body.
When the layers prior to the immune system are damaged, any substance, pathogen or not, is able to cross the barrier, activate the immune system and trigger an inflammatory response.
In these conditions (known as dysbiosis or leaky gut) not just viruses and bacteria, but also various other substances that are normally regarded as harmless, such as glucose, lactose, or substances produced by the body in response to stress or trauma (such as catecholamine adrenalin, noradrenalin or dopamine) are able to enter and can trigger an inflammatory response.
In fact, today we know that a chronic inflammatory process can be induced by psychological trauma, the environment, stress or nutrition.
As the gut continues to undergo damage, the body responds with an inflammatory process that, if unsolved, can become chronic, manifesting itself over time with a series of symptoms that range from allergic reactions to more serious diseases like cancer.
The most common causes for inflammation
Factors connected to gut dysfunction that typically create an environment favourable to a chronic inflammatory process are:
- Diet: gluten, casein, processed foods, sugar and carbohydrates, industrial food, fast food and so forth
- Drugs: corticosteroids, antibiotics, antacids etc
- Stress: an increase in cortisol (adrenaline, noradrenaline, dopamine)
- Emotional imbalance and trauma: stress alterations plus sympathetic-parasympathetic imbalance, vagal alteration, brain-networks etc
- Hormone imbalance: thyroid hormones, progesterone, oestradiol, testosterone
- At a neurological level: brain trauma, ictus etc
- Metabolic level: there are various processes, in particular glycosylate end products (inflammatory end products of sugar metabolism)
- Physical alterations: physical trauma, tissue lesion etc
- Infections: H-Pylori, yeast or bacterial proliferation, viral or parasite infection
- Cigarette smoke
- Alcohol abuse
- Endocrine disruptors (contained, incidentally, in detergents, soaps and various other household products).
In this article we look at nutrition and diet issues more in depth, for plenty more focus articles, explanation and practical suggestions on mental, emotional and physical aspects please see the various articles and videos on our blog or our online Integrative Sciences HUB courses.
PRO-INFLAMMATORY FOODS
The abundance of cheap, low-quality food that we find in supermarkets, accessible to everyone, certainly favours a number of metabolic processes that are negative for the human body.
Before providing a list of foods that can favour an inflammatory process, it is important to remember that we are not just talking about quality but also about quantity. In fact, a quantitative excess of food, both in terms of actual amounts and of intake frequency, is not good for overall health, regardless of the quality of the food.
Some of the foods that can cause dysbiosis, leaky gut and trigger an inflammatory process are:
- Sweet foods and sugary drinks: sweets, sodas, puddings, fruit juices, cakes etc that contain high quantities of fructose. Fructose metabolism produces toxic waste such as uric acid that leads to inflammation, endothelial damage, hypertension, gout and so on.
- Vegetable oils: cooking oils such as soy, maize, sunflower seed, palm etc. are rich in omenga-6. Too much omega-6 can trigger an inflammatory process producing prostaglandins, leukotrienes and thromboxane.

- Trans fats and fried foods: the chips, fish fingers and onion rings that we typically find in fast food outlets are often cooked in vegetable oils and are packed with trans fats.
- Refined carbohydrates: bread, pasta, pizza, focaccia, crackers, breadsticks and all flour products can favour an inflammatory process if consumed in excess. In addition to this, research has shown that wheat contains specific proteins called amylase trypsin inhibitors (ATIs) that can trigger an inflammation connected to chronic diseases such as multiple sclerosis, asthma and rheumatoid arthritis.
- Foods rich in glutamate and aspartame: excessive consumption of glutamate and aspartame favour chronic inflammation and connected diseases. Glutamate also tends to overstimulate cells causing damage to the brain on various levels and triggering or worsening learning difficulties, attention deficit, sleep disorders etc.
- Highly processed industrial foods.
How can you manage the inflammatory response to food?
A change in diet can certainly help to overcome an inflammatory process.
However, to favour change and recover physiological state it is not enough to increase some foods over others, but potentially inflammatory foods need to be limited or reduced.
It will therefore be useful to reduce or eliminate the following for a set period of time: carbohydrates such as pasta, bread or pizza, foods that contain fructose (soft drinks, fruit juices etc), all vegetable oils that contain high levels of omega-6, foods containing trans fats, foods rich in glutamate and aspartame.
We should:
Increase the intake of foods rich in omega-3 such as oily fish, meat from grazing animals that have mainly eaten grass or hay, free-range animal meat or free-range eggs.

Increase quality fats such as butter, eggs, oily fish like salmon, fatty matured cheese, cream, dark chocolate, dried fruit etc.
Increase intake of fibre-rich vegetables that contribute to the well-being of the gut microbiome.
And, after a period of preparation, introduce periods of intermittent fasting that are very useful to reduce inflammatory processes and favour a return to physiological state.
All these directions can be made all the more effective via exercises that help manage states of hyperactivation and hyperstimulation acting synergistically and systematically to reduce or overcome a chronic inflammation process. One example is the Crossed Cycles Breathing Technique that intervenes on different levels to manage stress responses, recover wellbeing, establish physiological state for body and mind and develop self-control in every situation.
In particular, carrying out this technique before meals enables a slow-down of rhythms and relaxes the mind and muscles in the top part of the body. It will thus be possible to eat calmly, enjoy out food and nourish ourselves in our physiological state both mentally and physically, creating ideal conditions to digest and absorb food.
Do you want to find out more about the nutrition-health connection?
Visit the online course THE KEY ROLE OF NUTRITION now.
Learn how to manage connections between nutrition, inflammation, emotions and psychosomatic disorders.
Do you want to find out more about the different features of inflammation?
Discover the many online courses on psychosomatic processes, regulation of anxiety and stress responses, emotion modulation, trauma and resistance to change. They are all part of the Integrative Sciences HUB, our regularly updated online training centre, available to you 24/7 with new COURSES, UPDATES, TECHNIQUES AND PRACTICAL TOOLS each month, all included in one subscription available at an annual fee of just 90€.
Stay connected with news and updates!
Join our mailing list to receive the latest news and updates from our team.
Don't worry, your information will not be shared.
We hate SPAM. We will never sell your information, for any reason.



